The de Tornyay Center for Healthy Aging was proud to see the impressive showing from the UW School of Nursing at this year’s Gerontological Society of America 2024 Annual Scientific Meeting. School of Nursing students, faculty, alumni and collaborators presented innovative work ranging from understanding unhoused older adults to technology, exercise and more at the event.
We look forward to seeing all the fruitful collaborations, research and connections that may come out of this exciting event. Read a few highlights from UW School of Nursing presentations at the conference below. Click on each title to see photos and short descriptions of highlighted presentations.
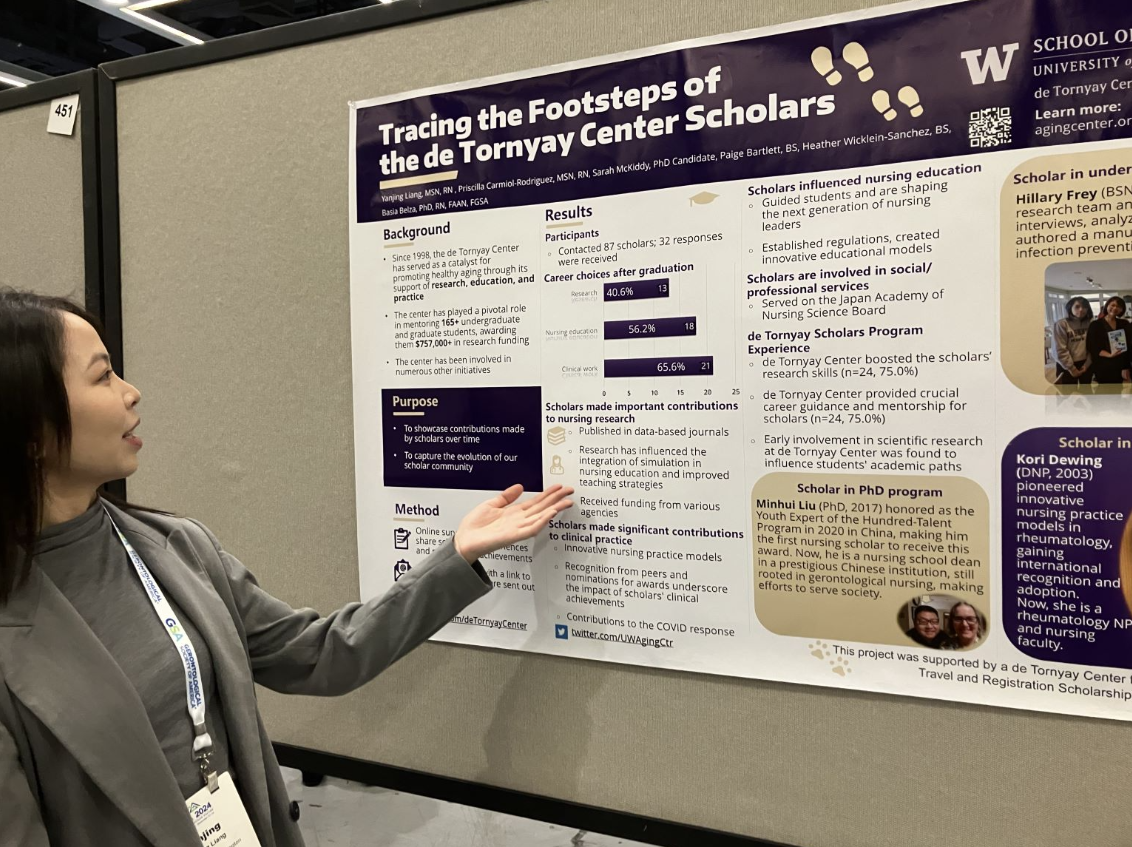
Since the de Tornyay Center for Healthy Aging opened its doors over 25 years ago, the center has funded over 165 scholars, giving out hundreds of thousands of dollars in student funding, said Yanjing Liang in a GSA poster presentation. Liang summarized the results of a survey of de Tornyay Center scholars in her poster, showcasing former scholars’ excellence in gerontological nursing research, practice, and leadership, helped in part by their time with the center.

The long-term care field across the U.S. is experiencing staffing shortages across the United States. Increasing the number of professionals in that industry is critical to caring for people with dementia. Associate Teaching Professor Kristen Childress presented a poster on nursing students’ reasons for not going into long-term care. Low wages and the lack of assistance with student loans were common reasons. Multiple students also felt that growing their career and skills in the long-term field would lead to administrative and supervisory work, when instead many wanted to grow their direct patient care skills and responsibilities, such as with a DNP. Students were also concerned about the working environment and mentioned the ratios of nurses to residents at long-term care facilities. The next step for Childress’ research is to study why people currently in the long-term care field choose this field.
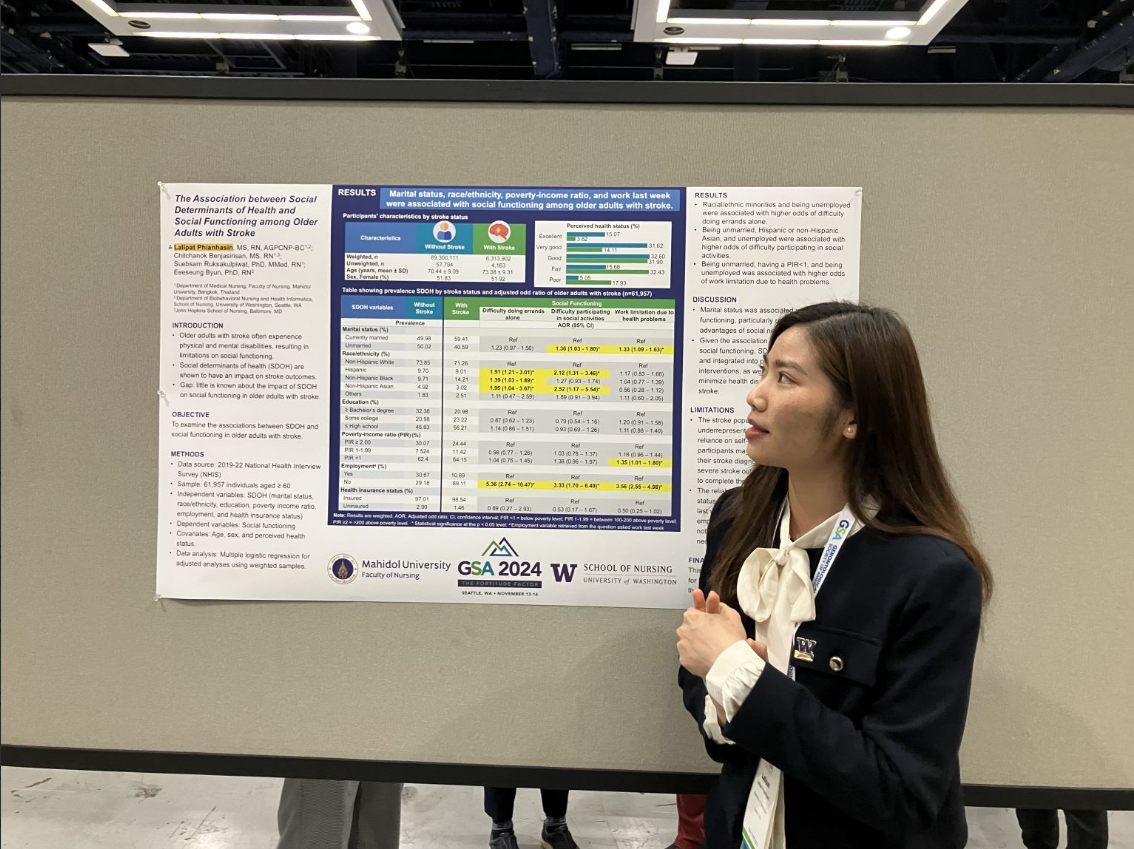
PhD student and de Tornyay Center illustrator Lalipat Phianhasin presented on social determinants of health in stroke recovery. Phianhasin and colleagues looked at factors — such as access to health care, socioeconomic status, race and education — to see how these factors, also known as social determinants of health, influence stroke recovery. Her work has turned up a number of connections. For example, being married helps with a number of aspects of recovery, such as having an easier time engaging with social activities.
Clinical Professor Anita Souza opened a panel on homeless older adults. She pointed to the fact that the proportion of unhoused older adults is growing and that people who are unhoused tend to experience “accelerated aging.”
Souza shared her recent study, using a statistical model to look at a homeless older adult population and find the statistical groups that exist within the homeless older adult population. The work pointed to key differences in sub-groups of the population, such as if they have health concerns and or substance use. In discussion, Associate Professor Jenny Tsai pointed out how the study demonstrates that this population is not a monolith. Different people in this population have different needs beyond just housing. UW DNP alumni Randee Robinson followed Souza and spoke about her project investigating barriers to accessing mental health care for residents at supportive housing. Robinson found many factors, like caseworker turnover, stigma and more, got in the way of mental health care. UW Medicine Clinical Assistant Professor Russel Berg shared cases from working at a hotel shelter with a medical clinic and psychiatric services, highlighting the many challenges of supporting older adults at the shelter.
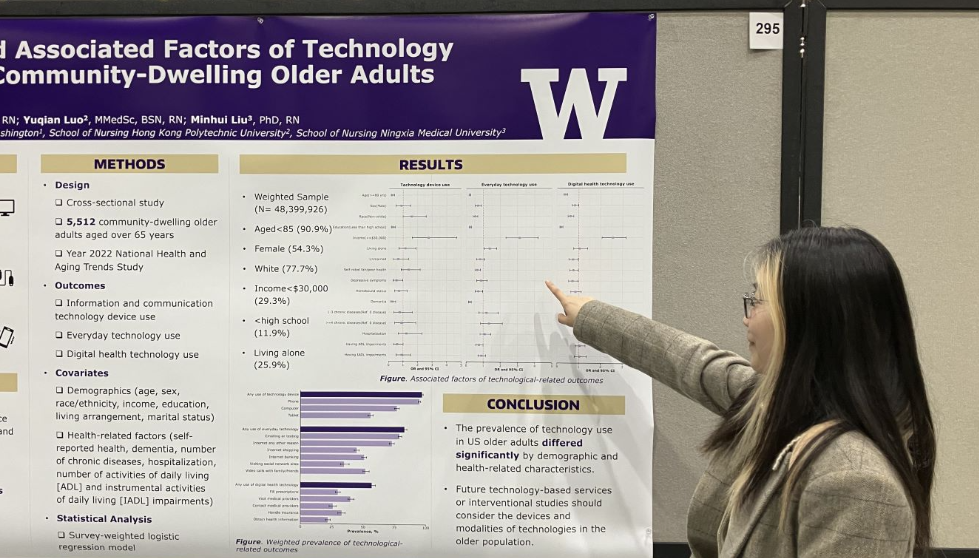
Since the COVID-19 pandemic, it’s becoming easier and more common to access health information online. PhD student and UW School of Nursing pre-doctoral scholar Wenting Peng investigated what older adults’ technology use currently looks like. Most older adults in the study data had a technology device, and a majority used technology every day. Fewer, but still more than half, use technology for health reasons. There were also major differences between older adults who did and didn’t use technology, both in general and for health purposes, with factors like gender, health and income all affecting how likely someone is to use digital health and commonplace technology.
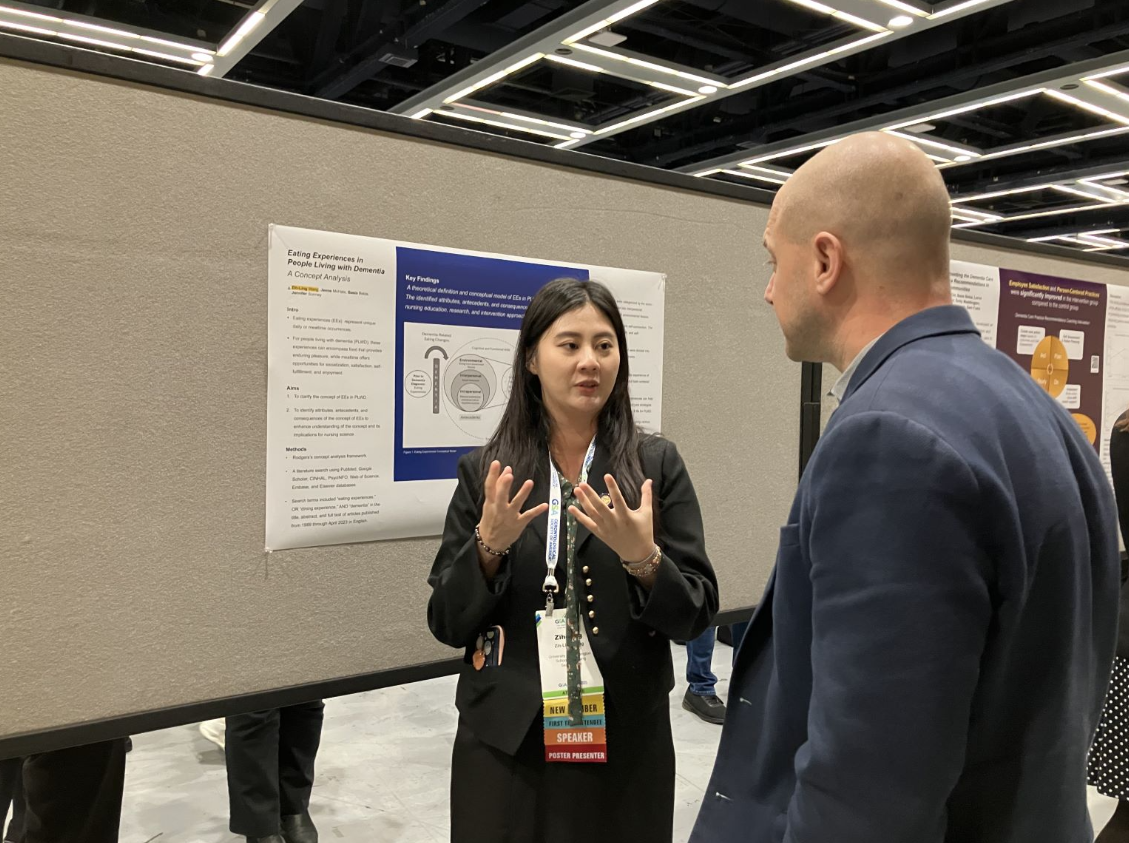
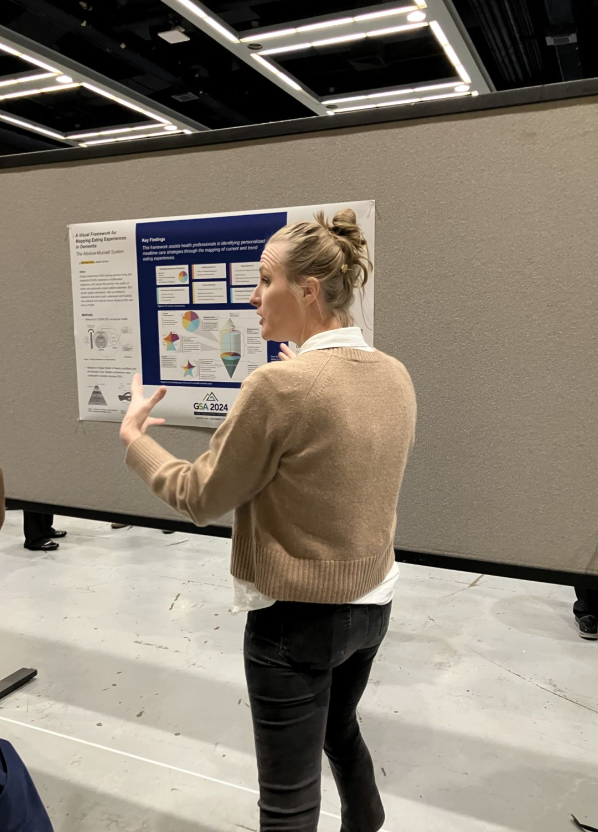
School of Nursing PhD student Zih-Ling Wang with fellow PhD student and co-author Jenna McHale presented on the experiences and challenges of eating with dementia. Examining the literature, they broke down eating experiences into environmental, interpersonal, and intrapersonal factors, as well as external and internal outcomes, such as nutrition and mental health. In another poster, the two students demonstrated how these ideas can be shown as a diagram of how dependent we are on others across the lifespan. We gain capabilities and dependence as we grow into adulthood, and tend to lose some of that independence toward the end of life. As the diagram they created shows, dementia can lengthen the amount of time an older adult has less independence, and make them lose independence earlier.
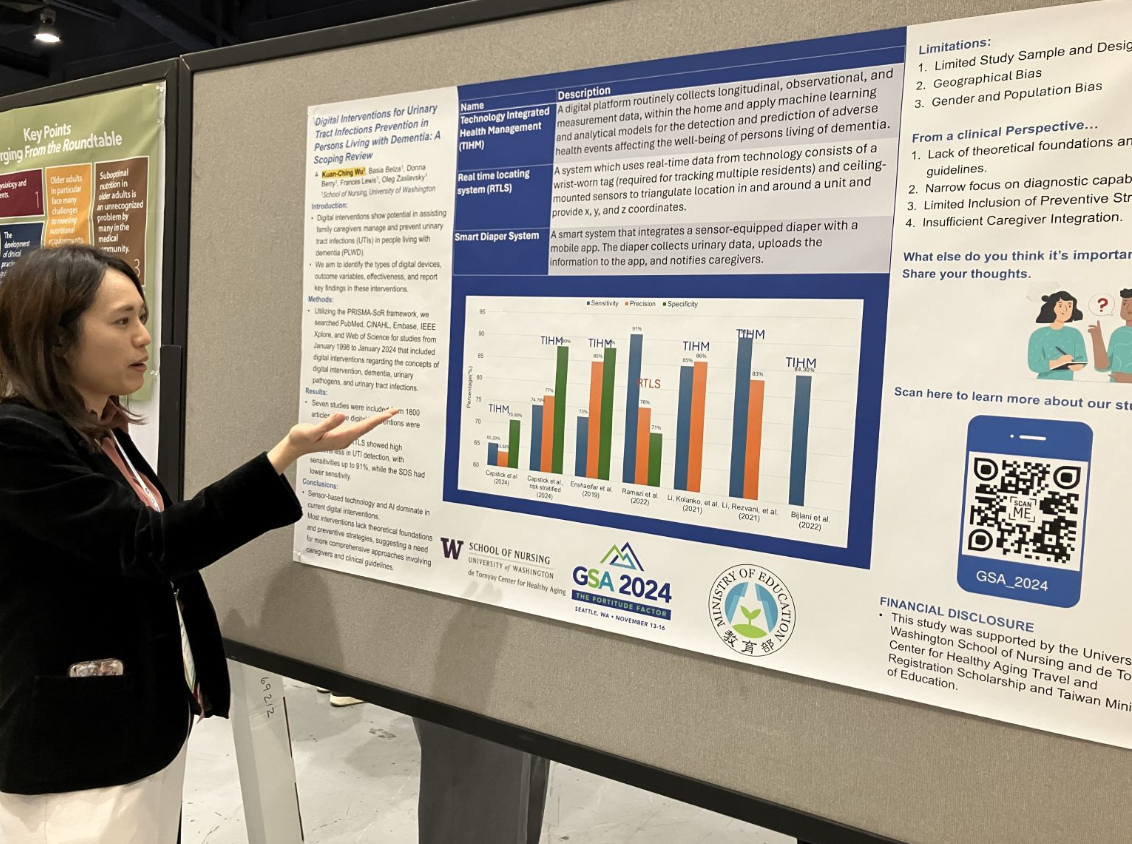
PhD student and former de Tornyay Center pre-doctoral scholar Kuan-Ching Wu presented her investigation of the current research on what interventions work for preventing urinary tract infections in people with dementia. The only three studies she found all focused on digital interventions, using technology like AI and sensors. The lack of work in this field points to the need for more robust support for people with dementia and their care partners to prevent UTIs. Interested in learning more about urinary tract infections in people with dementia? Read more in the de Tornyay Center’s Northwest Primetime article on UTIs and dementia, featuring Wu and her work.
Four PhD students presented deep dives into an array of research questions. The all-UW School of Nursing GSA session focused on something known as a ‘scoping review’, which is essentially a systematic review to get the big picture of the current research on a subject.
Mesh Otewa spoke about his scoping review on improving health equity in older adults, which is especially important as health disparities are increasing for older adults across a number of conditions. Otwea and colleagues found that studies on this topic tended to focus on technology (such as telehealth), improving access to health insurance (such as Medicaid), and making the healthcare system easier for older adults to navigate. One of the main takeaways from the scoping review was the importance of a practical approach to integrating new approaches into existing systems.
Jenna McHale presented a scoping review of eating behaviors and dementia, which was led by fellow PhD student Zih-Ling Wang. One of the key findings she presented was that “creating supportive dining environments” tended to be helpful for getting people with dementia to eat and drink more. McHale and Wang also found that there was a notable gap — not a lot of research focused on improving individuals’ ability to eat.
de Tornyaya Center pre-doctoral scholar Priscilla Carmiol-Rodriguez spoke about social frailty. As opposed to physical frailty, social frailty describes a lack of resources for meeting one’s social needs. While social frailty is common for older adults, it’s not studied much. Carmiol-Rodriguez’s study of the literature highlighted risk factors such as hearing loss, physical fraility, and other conditions. Social frailty, in turn, is connected with increased risk of conditions like poor mental health or cognitive impairment, as well as disability and quality of life. However, research shows that interventions can help. Things such as exercise, and improving older adults’ skill with technology have all been found helpful for socially frail older adults.
PhD student and former center pre-doctoral scholar Sarah McKiddy shared two scoping reviews in the panel discussion. Her first talk emphasized the diversity of current research on music interventions for people with dementia. Many focused on tailoring music to participants and their cultures. Some incorporated group elements and some included opportunities for community and socialization. Studies also differed on whether they had people participate in music, such as singing or playing an instrument, or just listening to it. Overall, she pointed to the need for standardized terms across the research to help the field distinguish between different types of treatments.
McKiddy’s second scoping review highlighted current research on group physical activity interventions for people with dementia and their care partners. These interventions can have many benefits, including both physical and mental health and general quality of life. When reviewing the research in her scoping review, McKiddy found that these benefits were reinforced across programs, although many people with dementia and their care partners often struggled with following exercise recommendations. More research could illuminate how to best tailor interventions to this population and their challenges.
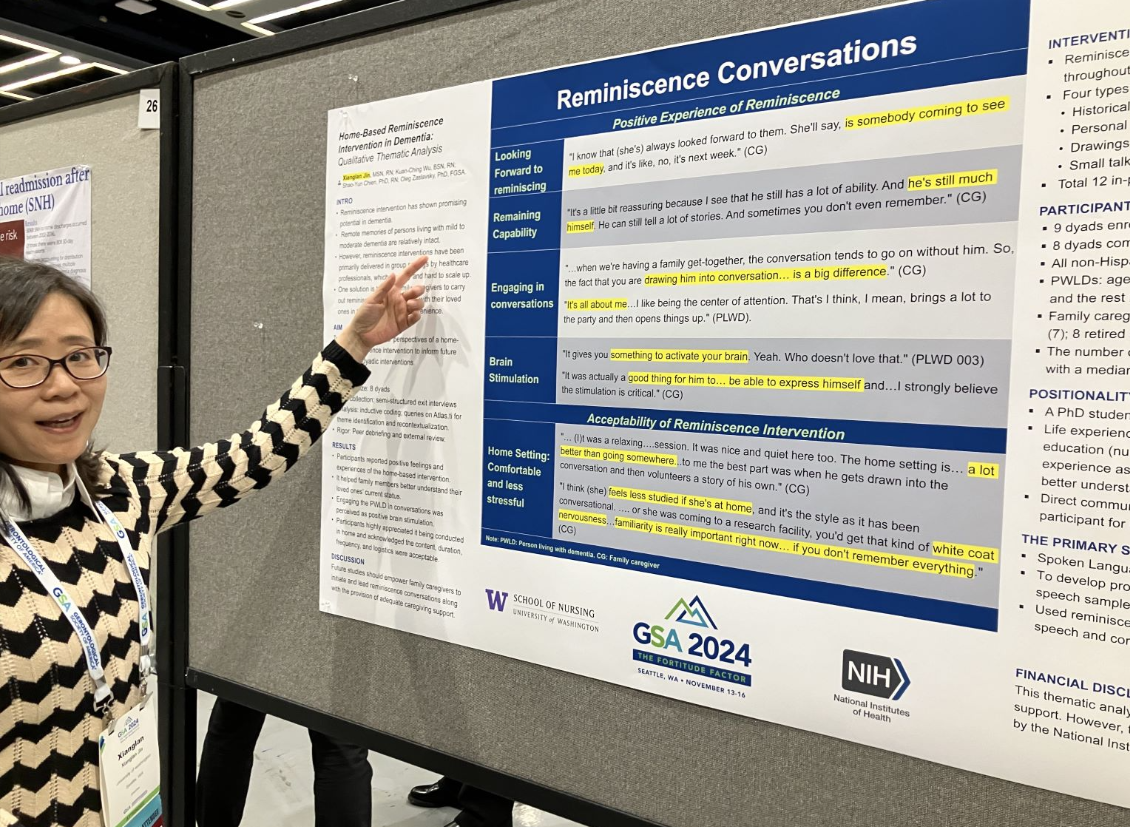
Encouraging people with dementia to think back on the past, or reminiscence, “has shown promising potential in dementia” says PhD student Xianglan Jin in the poster she presented at GSA. However, studies on reminiscing have mostly been in clinical and group settings, which makes it harder to spread widely. That’s why Jin and her colleagues set out to work with the care partners of people with dementia, to help teach them to deliver intentional reminiscence sessions with their loved ones, using photos, drawings, and chatting about life. Care partners shared that reminiscing was a wonderful way for their loved one to use their mind, and care partners enjoyed seeing just how much the person with dementia still remembered.
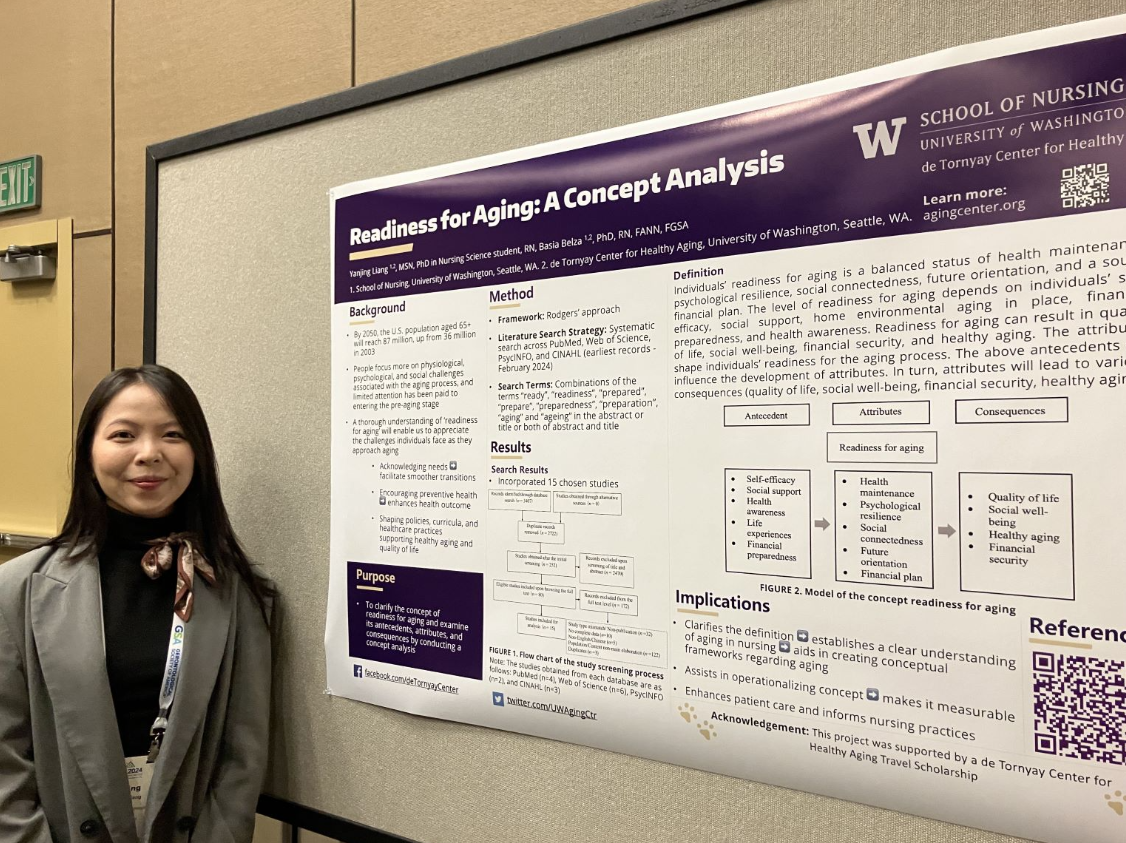
Understandably, there’s a lot of focus in gerontology on how older adults age well in their later years. But there’s been less emphasis on what we can all do earlier in life to prepare for older adulthood. PhD student and center pre-doctoral scholar Yanjing Liang presented her research investigating what makes up “readiness for aging”. Looking across 15 studies, she identified many factors, from social support to future plans, preparing financially, and so much more. This research provides a foundation for future study into how we can all best prepare for later life.
PhD student Suah Park investigated what makes up good sleep quality in older adults by reviewing the research paper on the topic. ‘Sleep quality’ includes a lot of different aspects, including how someone feels about their sleep, as well as more objective measurements, such as how long someone is asleep. The next steps for the research could include investigating the relationship between causes of good and poor sleep quality, the effects of sleep quality, as well as cases when subjective and objective measures of sleep quality are different, says Park.
Paige Dension, long-time collaborator with the UW School of Nursing and the director of Health, Wellness & Project Enhance at Sound Generations, introduced a panel on the EnhanceFitness program, which was established about 30 years ago in the Seattle area in collaboration with the University of Washington. Since then the program has been backed by an impressive array of evidence, continued through staffing changes at many organizations involved with the program, and has spread across the country to over 100 sites.
Fellow presenter and UW Medicine Research Professor Kushang Patel demonstrated that the program is still effective when delivered remotely, based on data collected during the COVID-19 pandemic. Building on that, University of Vermont Associate Professor Gell demonstrated the program worked well for cancer survivors going to the program virtually, and may have even helped attendance. UW Medicine Research Consultant Elise Hoffman highlighted barriers to getting participants referred to the program by their doctor, from the referral process being too complex to referrals dropping off over time. So her team developed an easy referral system for EnhanceFitness, where nurses can refer patients simply by selecting a class, and hitting a button that says ‘refer’.
de Tornyay Center Dr. Basia Belza shared a recent pilot study in the Seattle area by UW School of Nursing researchers looking at how feasible EnhanceFitness was for people with dementia and their care partners. The study aimed to understand how best to adjust the programming to the population. There were many barriers to attendance, with 6 out of 8 of the pairs of participants dropping out of the study. Reasons ranged from unrelated health problems to being too tired and more. Overall, the study points to areas for improvement to help make the program accessible to this population.
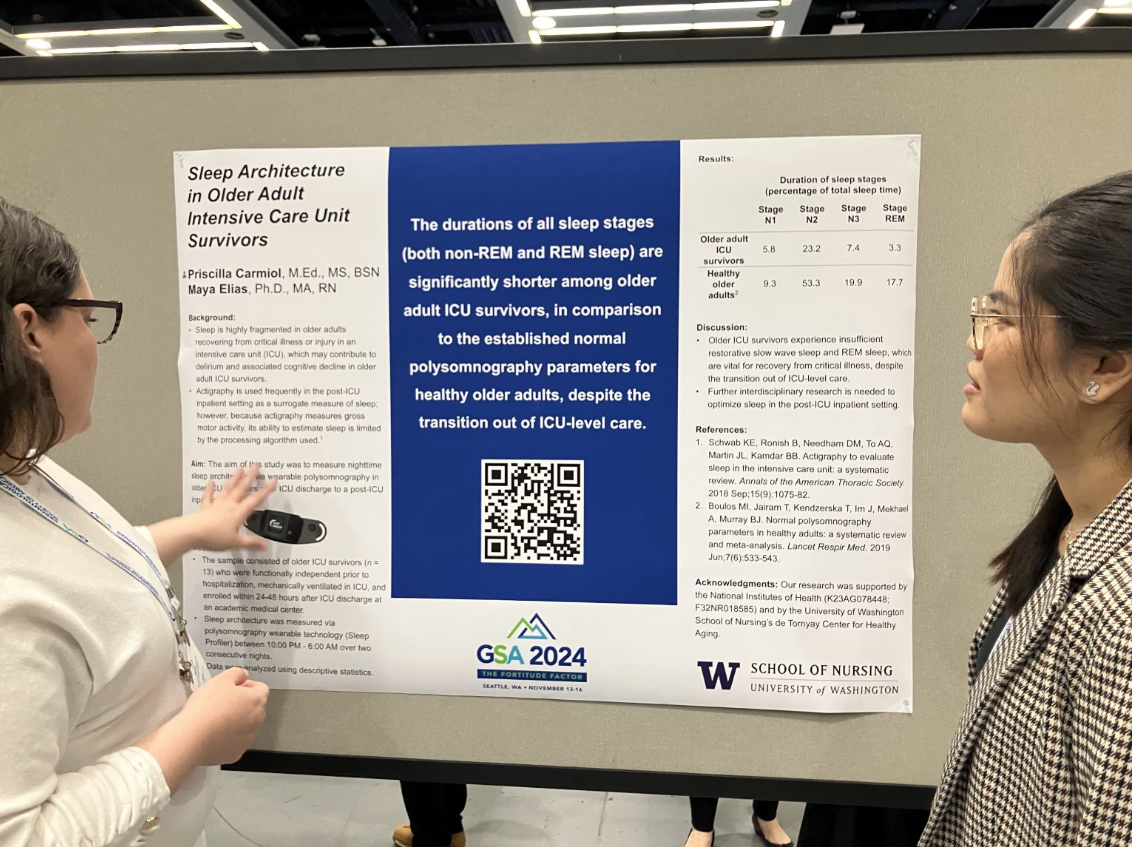
Priscilla Carmiol-Rodriguez presented data investigating sleep in ICU survivors, once they were discharged from the ICU into less intensive hospital environments. She found that across the board participants’ sleep was negatively impacted. Compared to healthy adults they spent less time in each of the different stages of sleep – from light sleep, deep sleep, and REM (the stage when we dream). The reason? They were sleeping much less throughout the night. The hospital environment, as well as their health, both might be affecting sleep said Carmiol-Rodriguez. One potential solution could be narrowing the window when hospital staff will wake a patient up. Interestingly, Carmiol-Rodriguez shared that after a hospital stay, some research shows people may continue to sleep poorly after an ICU stay for as long as a year.
The CDC has a robust set of recommendations to help prevent falls for older adults. Their STEADI program has information for everyone from hospitals to pharmacists, Executive Dean Hilaire Thompson shared, when presenting a poster on an adaption of the program. However, nothing similar exists for long-term care. So Thompson and colleagues set out to adapt STEADI for the long-term care setting. They spoke to staff at facilities and to experts to get an idea of what might be feasible and best practice. As a result of her team’s efforts, the STEADI-LTC care program is currently being tested at facilities around Western Washington. The researchers are keeping an eye on many factors, from if the program reduces falls to what aspects of the program long-term facilities do and don’t implement.